Cholesterol and Inflammation – the article discusses common misconceptions about the role of cholesterol and presents the truth about the real impact of triglycerides and inflammation.
Cholesterol is Essential – Low Carb, Keto Diet by Annika Urm
Annika Urm Health School publishes evidence‑based, scientifically supported information about cholesterol. In this article, common misconceptions about the role of cholesterol are discussed, and the truth about the real impact of triglycerides and inflammation is explained.
The article emphasizes the necessity of distinguishing between different types of cholesterol and their respective effects on vascular health. It asserts that while cholesterol is often vilified, it plays a critical role in bodily functions, and that elevated triglyceride levels and chronic inflammation are more significant contributors to vascular disease. By addressing these issues, the article aims to foster a more nuanced understanding of heart health, encouraging readers to consider dietary strategies that prioritize controlling inflammation and managing triglyceride levels for optimal wellness.
How Does LDL “Bad” Cholesterol Save Your Life?
Cholesterol plays an essential role in maintaining overall health, yet it is often misunderstood merely as a risk factor for heart disease. In reality, cholesterol is indispensable for hormone production, vitamin D synthesis, and maintaining the integrity of cell membranes. Keto and low‑carbohydrate (Low Carb) diets not only help improve cholesterol markers but also reduce inflammation and triglyceride levels, thereby supporting cardiovascular health. Discover the science behind cholesterol and learn how to find the right balance for a healthier life.
This article explains the roles of LDL and HDL in the body and why the division into “good” and “bad” cholesterol must be viewed in a broader context.
Cholesterol is an essential substance for the human body, whose role extends from supporting cellular functions to maintaining hormonal balance. Although LDL cholesterol is often considered “bad,” its function in repairing blood vessel damage is vital.
Cholesterol is also critical for repairing blood vessel damage. Instead of focusing solely on lowering LDL cholesterol levels with medication, it is necessary to understand the biological importance of cholesterol and direct attention toward preventing inflammation and metabolic disorders.
Nutrition and Keto Specialist Annika Urm, who is a specialist in keto and Low Carb nutrition and therapeutic nutrition, explains in this article the roles of good and bad cholesterol and triglycerides and shares valuable advice on how to eat healthily and improve your health yourself through food. Food is your best medicine.
Food is your best medicine.
The Role of Cholesterol in the Body
Cholesterol is a central and necessary substance for normal bodily functions. Its main functions include:
- Building cell membranes: Cholesterol ensures the stability and flexibility of cell membranes.
- Hormone synthesis: Important hormones are produced from cholesterol, including sex hormones (estrogen, testosterone) and cortisol.
- Vitamin D production: Vitamin D is synthesized from cholesterol and is necessary for bone health and immunity.
- Bile acid production: Bile acids are formed from cholesterol and are important for fat digestion.
- Nervous system function: Myelin sheaths, which surround and protect nerves, contain large amounts of cholesterol.
- Antioxidant protection: Cholesterol helps protect cells from damage caused by free radicals.
- Cell signaling mechanisms: Cholesterol participates in communication between cells.
- Support of immune function: Cholesterol regulates inflammation and supports immune responses.
- Transport of lipids and vitamins: Cholesterol stabilizes lipoproteins that transport fats and fat-soluble vitamins.
- Cell renewal and repair: Cholesterol is critical for cell proliferation and tissue repair.
Cholesterol moves in the blood via lipoproteins, including LDL (low-density lipoprotein) and HDL (high-density lipoprotein).
The Vascular Repair Theory – LDL (low-density lipoprotein) as a “firefighter” rushing to the scene to extinguish the fire
When blood vessels are damaged (for example due to inflammation, toxins, or free radicals), the body uses LDL and cholesterol to repair these “fires” or “holes.” This explains why higher LDL (low-density lipoprotein) may sometimes reflect the body’s natural response to vascular stress or damage rather than a pathological condition.
LDL (low-density lipoprotein) – “bad” cholesterol or indispensable?
LDL cholesterol is often called “bad” cholesterol because its oxidized form is associated with the development of atherosclerosis. In reality, LDL (low-density lipoprotein) is indispensable in the body and fulfills several important functions.
Why is LDL (low-density lipoprotein) necessary?
How does LDL (low-density lipoprotein) help repair blood vessels?
- Cholesterol transport: LDL carries cholesterol from the liver to tissues where it is used for cell and hormone production.
- Endothelial repair: LDL helps deliver cholesterol to damaged blood vessel walls in order to repair and strengthen them.
- Cell stabilization: Lipids delivered via LDL support cellular integrity and functionality.
LDL (low-density lipoprotein) as the body’s repairer
One of the main functions of LDL is to supply cholesterol and other lipids to tissues, including the vascular endothelium. When the blood vessel wall is damaged (for example due to inflammation, high blood pressure, or toxins), LDL is sent there for “repair work.” This is a natural and necessary response of the body.
Why is LDL (low-density lipoprotein) “blamed” for disease?
Although LDL participates in blood vessel repair, it becomes the “primary cause” when the following conditions are present:
- Chronic damage: If the vascular endothelium is constantly damaged (for example due to chronic high blood pressure, smoking, or diabetes), the body must continuously send LDL there. This leads to LDL accumulation in the vessel walls.
- Oxidative stress: When LDL enters an inflammatory environment, it becomes oxidized. Oxidized LDL no longer fulfills its repair function but instead triggers an immune response that initiates the atherosclerotic process.
- Inflammation and immune response: Oxidized LDL attracts immune cells (such as macrophages), which “ingest” the oxidized LDL and become foam cells. The accumulation of foam cells forms plaque and narrows blood vessels.
LDL (low-density lipoprotein) is not the problem, but a symptom
LDL itself does not cause disease. Its primary task is to help repair damaged tissues. The problem arises when damage is chronic and inflammatory and when the body lacks a balancing mechanism to control inflammation.
Important focus: why do blood vessels become damaged?
Instead of focusing solely on lowering LDL (low-density lipoprotein) levels, emphasis should be placed on maintaining vascular health and preventing damage:
- Reducing chronic inflammation: Balanced nutrition and lifestyle that reduce inflammatory markers (for example CRP).
- Preventing oxidative stress: Antioxidant-rich foods, regular physical activity, and smoking cessation.
- Controlling blood pressure and blood sugar: These reduce vascular stress and endothelial damage.
LDL (low-density lipoprotein) as the body’s natural “repairman”
The role of LDL in repairing vascular damage is vital. Problems arise when vascular damage is chronic and an inflammatory environment causes LDL to become oxidized, leading to pathological processes. Therefore, instead of searching for a culprit, focus should be placed on improving vascular health and reducing inflammatory factors.
LDL oxidizes mainly due to free radicals and oxidative stress, especially in a damaged vascular environment. Preventing this process depends on a healthy lifestyle, adequate intake of antioxidants, and control of inflammatory processes. By avoiding oxidation, the risk of atherosclerosis can be reduced and vascular health supported.
LDL cholesterol oxidation and inflammation are directly related to the vascular repair process, in which LDL participates in the “repair” of endothelial damage. However, if the environment at the site of damage is toxic or inflammatory, this natural repair process can become pathological, leading to the development of atherosclerosis.
Atherogenic processes– Atherogenic refers to processes, factors, or substances that promote the development of atherosclerosis. Atherosclerosis is a chronic vascular disease in which lipids (such as cholesterol) accumulate in the arterial walls, causing inflammation, narrowing, and stiffening of blood vessels. This can lead to cardiovascular diseases such as heart attack, stroke, and the development of peripheral arterial disease.
HDL (high-density lipoprotein) – “good cholesterol” and its importance
HDL transports excess cholesterol from tissues back to the liver, where it is removed or reused. This process is also called “reverse cholesterol transport” and helps keep blood vessels healthy. Low HDL does not automatically indicate a problem, but high HDL levels may indicate better lipid balance and overall metabolic health. However, it is important to view HDL as part of the overall picture, not as the sole health indicator.
Triglyceride is a blood fat – an important marker. NB! It must be monitored!!!
Triglycerides are the most important blood fat marker, and their level often rises with high carbohydrate intake and insulin resistance. Triglycerides are directly related to metabolic health, and monitoring their levels helps assess cardiovascular disease risk.
High triglycerides indicate: metabolic syndrome, insulin resistance, and increased cardiovascular disease risk.
The role of insulin: High insulin levels associated with frequent carbohydrate-rich eating block fat burning and promote the accumulation of triglycerides in the blood.
The most accessible treatment for every person is a low-carbohydrate, or ketogenic, diet.
Keto and low-carbohydrate diets promote the reduction of inflammation and the lowering of triglyceride levels in the blood through multiple mechanisms. Limiting carbohydrate intake reduces insulin levels, which in turn decreases systemic inflammation and oxidative stress. In addition, the state of ketosis stimulates the breakdown of fats for energy, thereby reducing triglyceride concentrations in the blood. A high intake of healthy fats combined with moderate protein consumption also helps stabilize blood glucose fluctuations, which is important for reducing inflammatory markers. Through the combined effect of these mechanisms, the lipid profile improves and the risk of cardiovascular disease decreases.
Healthy and Delicious Keto Low Carb Baking Mixes Created by Annika Urm
Discover the Keto and Low Carb baking mixes created by Annika Urm, which are healthy, delicious, and perfectly suited to your dietary plan! Each slice contains only 1–2 g of carbohydrates, while being rich in beneficial fiber and healthy fats. Annika uses carefully selected ingredients in her recipes that are often found in health supplement capsules: psyllium husk, konjac root (glucomannan powder), omega-3, and flaxseed oil.
Food Is Your Fuel!
Nutrition is the foundation of a healthy lifestyle. If you care about your health, choose Annika Urm’s baking mixes, which are:
- Gluten-free
- Sugar-free
- Low Carb and Keto friendly
An ideal choice for people with diabetes and health-conscious individuals!
Bread mixes and much more!
24 Different Golden Stevia Keto Baking Mixes – Sugar-Free, Low Carb & Diabetic Friendly
Discover 24 different Golden Stevia Keto & Low Carb baking mixes, designed for a ketogenic, low-carbohydrate, and sugar-free lifestyle. Perfect for people with diabetes, insulin resistance, cardiovascular concerns, and health-conscious consumers.
🥖 Keto Bread & Savory Baking Mixes
- Hemp Bread Mix
- Golden Flaxseed Bread Mix
- Brown Flaxseed Bread Mix
- Pumpkin Seed Bread Mix
- Psyllium Husk Baguette Mix
- Keto Almond Bread Mix
- Crunchy Golden Keto Bread Baking Mix
- Crunchy Black Keto Bread Baking Mix
- Keto Hemp Cracker Mix
- Keto Cracker Omega-3 Mix
- Keto Burger Bun Baking Mix
🧁 Keto Muffin Mixes
- Keto Chocolate Muffin Mix
- Keto Almond-Cinnamon Muffin Mix
🥞🍕 Keto Everyday Baking Mixes
- Keto Pancake Mix
- Keto Pizza Crust Mix
- Keto Cinnamon Buns Mix
- Keto Cake Baking Mix
🍪🌮 Keto Cookies, Pastry & More
- Keto Almond Cookie Mix
- Keto Cranberry-Flaxseed Cookie Mix
- Keto Tortilla & Taco Mix
- Keto Shortcrust Pastry Baking Mix
🥣 Keto Muesli
- Keto Muesli Strawberry Coconut
- Keto Muesli Chocolate Nuts
✅ Why Choose Golden Stevia Keto Products?
- Sugar-Free
- Low Carb & Keto Friendly
- Diabetic Friendly
- Gluten Free
- Sweetened with Natural Stevia, Monk Fruit & Erythritol
- Includes Keto Bread Mixes, Pizza, Pancakes, Muesli & Shirataki Pasta/Rice
- Easy to make at home
@goldenstevia #cholesterol #carnivore #annikaurm#cookbook#keto#lowcarb#ketobread#ketobaking #sugarfree#suhkruvaba#insulin#diabetes#arthritis #cardiovascular #tervis #cancer #arst#nurse#lowcarbshop#toitumisnõustaja #tervis#tervisliktoitumine #vitamins #alzhaimer #diabeet
www.goldenstevia.com
All These Products and More Are Available in the Golden Stevia Online Shop
👉 Baking Mixes – Golden Stevia
👉 Bread Mixes – Golden Stevia
Quick and Easy to Prepare
By ordering Golden Stevia baking mixes, you can easily prepare healthy, sugar-free, Keto and Low Carb products at home. Order ready-made breads or baking mixes and enjoy delicious and healthy nutrition every day.
Give Your Body the Best Fuel
Choose Annika Urm’s functional nutrition, designed to support your health and perfectly suited for people with diabetes as well as healthy individuals. These products are created to fit a Keto, Low Carb, and sugar-free lifestyle.
👉 Try them now and order here: Golden Stevia Baking Mixes
💚💛YOUR LOW-CARB KETO ONLINE SHOP!💚💛
💚💛DELIVERY ALL OVER EUROPE& UK 💚SPAIN, ITALY, GERMANY, FRANCE, POLAND, HOLLAND💛
✅ SUGAR-FREE, LOW-CARB, KETO
✅DIABETIC FRIENDLY
✅ GLUTEN FREE
💚💛 24 DIFFERENT KETO BAKING MIXES
EASY TO MAKE AT HOME
💚💛 NATURAL STEVIA, MONK FRUIT, ERYTRITHOL SWEETENERS
💚💛 SHIRATAKI PASTA, RICE
💚💛 KETO MUESLI
💚💛 LOW CARB KETO BREAD MIXES, PIZZA, PANCAKES ETC
👇👇👇👇
ORDER NOW
FAMILY BUSINESS 10 YEARS KETO, LOW CARB AND DIABETES EXPERIENCES
The Relationship Between LDL (Low-Density Lipoprotein) and Triglycerides
LDL (low-density lipoprotein) and triglycerides are closely interconnected. When triglyceride levels are high, this often indicates a predominance of small, dense LDL particles. These particles are more atherogenic and are strongly associated with atherosclerosis and vascular damage.
Conversely, when triglyceride levels are low and HDL levels are high, this typically indicates larger, more buoyant LDL particles, which are less atherogenic and may reflect a healthier lipid profile.
Is “Higher LDL” Actually Healthy?
“Larger” refers to physically larger and lighter LDL particles, as opposed to smaller and denser LDL particles. The health impact of LDL depends largely on accompanying factors such as HDL levels, triglyceride levels, and the presence of inflammatory markers.
When Can High LDL Indicate Good Health?
High LDL may be a sign of good health when:
- HDL levels are high and triglycerides are low
This indicates balanced lipid metabolism and minimal inflammatory activity. - Inflammatory markers such as C-reactive protein (CRP) are low
Low inflammation markers suggest healthy blood vessels and the absence of chronic inflammation. - Metabolic markers are optimal
Good insulin sensitivity, stable blood glucose, and normal blood pressure indicate metabolic balance and reduce the harmful impact of LDL.
When Is High LDL Harmful?
LDL becomes harmful under the following conditions:
Chronic inflammation
Persistent inflammation damages the vascular endothelium, creating an environment conducive to LDL oxidation. Oxidized LDL triggers inflammatory cascades that lead to atherosclerosis.
Insulin resistance
Poor insulin sensitivity increases triglyceride levels, causing LDL particles to become smaller and denser. These small, dense LDL particles are the most atherogenic and strongly promote plaque formation.
High oxidative stress
An excess of free radicals leads to LDL oxidation. Oxidized LDL loses its natural transport function and instead provokes immune reactions and inflammation.
Elevated inflammatory markers (e.g., CRP)
High CRP levels indicate active inflammation, increasing the risk of vascular damage and atherosclerosis.
Atherogenicity is therefore not caused by LDL or cholesterol alone, but by a broader combination of inflammation, oxidative stress, and metabolic dysfunction. A holistic approach to vascular health is essential.
LDL Oxidation and the Role of Inflammation in Vascular Health
LDL cholesterol plays a role in repairing vascular damage by helping restore endothelial integrity. However, when the repair site exists in an inflammatory or oxidative environment, this natural repair mechanism becomes pathological, leading to atherosclerosis and chronic vascular disease.
Main Atherogenic Factors
Oxidized LDL cholesterol
Oxidized LDL damages the endothelium, triggering inflammation and plaque formation. Continuous vascular injury causes repeated LDL accumulation, narrowing arteries and forming plaques.
High triglyceride levels
Associated with small, dense LDL particles, which are significantly more atherogenic and greatly increase atherosclerosis risk.
Inflammation and insulin resistance
Markers such as CRP reflect vascular inflammation and progressive damage. Insulin resistance and diabetes accelerate small LDL particle formation and vascular injury.
Smoking and hypertension
Smoking increases LDL oxidation and vascular inflammation. High blood pressure creates constant mechanical stress on vessel walls, accelerating plaque formation and arterial stiffness.
Low HDL cholesterol
Low HDL levels impair cholesterol removal from vessel walls, increasing atherosclerosis risk.
The Role of Hyperglycemia in Vascular Damage (Diabetes, High Blood Sugar)
Hyperglycemia exerts multiple harmful effects on blood vessels and promotes atherosclerosis through:
- Inflammation – High blood glucose activates inflammatory pathways that damage the endothelium and promote LDL oxidation.
- Oxidative stress – Increased free radical production damages vascular structures and accelerates aging.
- Glycation – Chronic high glucose leads to protein and lipid glycation, stiffening blood vessels and increasing susceptibility to inflammation and oxidation.
Chronic hyperglycemia weakens HDL’s protective role and increases LDL oxidation, making glucose control critical for vascular health.
The Atherogenic Process
- Endothelial damage (from hypertension, inflammation, toxins)
- LDL accumulation and oxidation
- Inflammatory immune response and foam cell formation
- Plaque instability, thrombosis, heart attack, or stroke
LDL oxidation and inflammation are the root causes of atherosclerosis. Risk is amplified by high triglycerides, smoking, insulin resistance, and low HDL.
Practical Steps to Support Health: Nutrition and Lifestyle
Rather than focusing solely on lowering LDL, the priority should be reducing inflammation and oxidative stress, which are the true drivers of vascular disease.
Diet affects cholesterol levels by only about 15%, as most cholesterol is produced by the liver. Problems arise when cholesterol is combined with carbohydrates, which raise insulin and promote inflammation. Fat combined with stevia or monk fruit does not raise insulin and allows fat to be efficiently utilized for energy.
Nutrition
Low-carb and ketogenic diets
Reduce insulin resistance and inflammation, stabilize blood sugar and triglycerides, increase HDL, and reduce small LDL particles.
Omega-3 fatty acids
Sources include fatty fish, flaxseed, and walnuts. Omega-3s reduce inflammation and support vascular health.
Avoid processed carbohydrates and sugars
They spike insulin and promote inflammation. Choose low-glycemic carbohydrates instead.
High fiber intake
Sources include vegetables, shirataki noodles, 100% fiber rice (prebiotic), psyllium husk, and keto breads made from seed flours (flax, hemp, pumpkin seeds).
Golden Stevia bread mixes – sugar-free, gluten-free, GMO-free, low-carb, healthy, easy to prepare and purchase.
Lifestyle
Quit smoking and avoid toxins
Smoking increases oxidative stress, LDL oxidation, and vascular inflammation.
Physical activity
Improves insulin sensitivity, lowers CRP, and raises HDL cholesterol.
Stress management
Chronic stress raises cortisol, worsening inflammation and insulin resistance. Meditation, yoga, and quality sleep are essential.
Antioxidants
Vitamin C, vitamin E, polyphenols (turmeric, green tea, berries) reduce oxidative stress and support vascular health.
Lifestyle changes—especially low-carb and ketogenic nutrition—are the most effective first-line intervention. Targeting LDL alone with medication without addressing inflammation has limited benefit.
Cholesterol and Eggs – Myth or Truth?
Eggs are one of the most nutrient-dense foods, providing high-quality protein, healthy fats, and essential micronutrients. Dietary cholesterol has minimal impact on blood cholesterol, contributing only about 15%. Eggs do not increase cardiovascular risk in healthy individuals.
Problems arise when cholesterol-rich foods are combined with carbohydrates, which raise insulin and inflammation. Low-carb diets keep insulin low, allowing fats to be efficiently used for energy and reducing chronic inflammation.
Why Eggs Combined with Carbohydrates Are a Problem
- Increased liver triglyceride production
- Formation of small, dense LDL particles
- Increased inflammation and LDL oxidation
Best Ways to Eat Eggs
- Combine eggs with low-carb foods: vegetables, avocado, keto bread
- Avoid pairing eggs with sugar or refined carbohydrates
- East eggs with stevia and monk fruit – Golden Stevia shop has the best keto sweetners in Europa
Eggs are healthy. The issue is not the egg, but the dietary context. Cholesterol becomes harmful only in a high-carbohydrate, high-insulin environment.
Carbohydrate Intake and Metabolic Health
Balanced nutrition means reducing carbohydrates to around 50 g per day.
Ketogenic diets reduce carbs to 20–30 g per day.
Low-carb diets range from 30–120 g per day, depending on body weight and goals.
Modern diets often exceed 250–300 g of carbohydrates per day, far beyond what the human body is adapted to process.
Reducing carbohydrate intake improves insulin sensitivity, lowers inflammation, supports metabolic health, and reduces cardiovascular risk.
Annika Urm highlights several highly important points that are aligned with many contemporary scientific studies.
Carbohydrate Reduction – A Key Factor in Metabolic Balance
Reducing carbohydrate intake to approximately 50 grams per day is a highly effective step, especially for individuals aiming to improve insulin sensitivity, reduce inflammation, and support overall metabolic health. This level is closer to the natural carbohydrate tolerance of the human body, which many researchers consider optimal for maintaining a healthy body weight and hormonal balance.
Ketogenic Nutrition (20–30 g of carbohydrates per day)
A ketogenic diet, where carbohydrate intake is reduced to 20–30 grams per day, is extremely effective in situations such as diabetes management, weight loss, and inflammation reduction. The ketogenic state enables the body to use fat as its primary energy source, which lowers insulin levels and allows the body to burn fat stores more efficiently.
Modern Carbohydrate Consumption – A Major Problem
Today, many people consume 250–300 grams or more of carbohydrates per day, largely due to processed foods and sugar-rich diets. The human body, which has evolutionarily adapted to process much smaller amounts of carbohydrates (primarily from vegetables, seasonal fruits, and some whole foods), is not capable of efficiently managing such excess intake.
This leads to:
- Chronically elevated insulin levels
- Insulin resistance
- Weight gain and diabetes
- Increased risk of cardiovascular disease
The Human Body Is Not Designed for Excessive Carbohydrate Intake
From an evolutionary perspective, carbohydrate sources were primarily natural foods such as vegetables and seasonal fruits, which were not consistently available year-round. Refined carbohydrates and added sugars are a modern dietary phenomenon, and their impact on metabolic health is largely negative.
You can find Annika Urm’s science-based research article here:
Science-Based Analysis of Low-Carb and Ketogenic Nutrition:
The Most Effective Treatment for Many Diseases, Including Diabetes
KETO NUTRITION
How Does a Ketogenic Diet Reduce Inflammation and Insulin Resistance?
The ketogenic diet (a low-carbohydrate, high-fat diet) positively and effectively influences metabolic processes through which inflammation and insulin resistance are reduced. The keto diet optimizes energy utilization and improves cellular function, including mitochondrial health and efficiency.
1. Reducing Insulin Resistance Through a Ketogenic Diet
Fewer carbohydrates, less insulin production:
A ketogenic diet lowers blood glucose levels, which in turn reduces the need for insulin. Low insulin levels improve cellular insulin sensitivity, helping to alleviate insulin resistance.
Triglyceride and fatty acid metabolism:
The ketogenic diet promotes fat burning, reduces triglyceride levels, and improves the lipid profile, thereby supporting metabolic balance.
Stable blood glucose levels:
Without sharp blood sugar fluctuations, the body can more easily regulate inflammation and stress levels.
2. Reducing Inflammation Through a Ketogenic Diet
Fewer inflammation-induced free radicals:
A ketogenic diet reduces glucose-based energy production, which is associated with increased free radical formation. Energy production from fatty acids and ketone bodies is “cleaner” and generates less oxidative stress.
Anti-inflammatory effects of ketone bodies:
Ketone bodies, especially β-hydroxybutyrate, are naturally anti-inflammatory and reduce inflammatory markers such as CRP (C-reactive protein).
Impact on the gut microbiome:
A ketogenic diet helps balance the gut microbiome, reducing inflammation-related endotoxin leakage into the bloodstream.
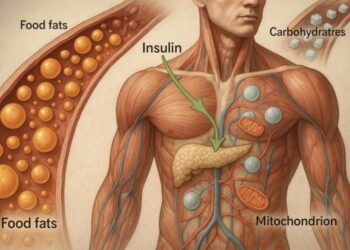
Mitochondria and Their Crucial Role in Energy and Inflammation Regulation
Mitochondria are the “power plants” of cells, producing energy (ATP) and playing a critical role in cellular metabolism. Their health and quantity directly affect inflammation, insulin sensitivity, and overall energy production.
1. The Role of Mitochondria in Reducing Inflammation
Clean energy production:
Efficient mitochondria produce energy without excessive free radicals, reducing oxidative stress.
Regulation of intracellular inflammation:
Mitochondria regulate inflammatory and anti-inflammatory signaling within cells, maintaining balance.
2. Effects of a Ketogenic Diet on Mitochondrial Health
Optimized energy production:
A ketogenic diet promotes mitochondrial energy production from fatty acids and ketone bodies, which is more efficient and less inflammatory than glucose-based energy.
Mitochondrial biogenesis:
During a ketogenic diet, the number of mitochondria increases as the body adapts to producing energy via fat oxidation.
Reduced mitochondrial dysfunction:
Ketones help stabilize mitochondrial membranes and improve their function.
How to Increase Mitochondrial Number and Efficiency
To improve mitochondrial quantity and function, ketogenic nutrition should be combined with other lifestyle strategies.
Physical activity:
Aerobic exercise:
Increases mitochondrial number and capacity.
HIIT (High-Intensity Interval Training):
Intense training stimulates mitochondrial biogenesis and improves function. It also promotes the release of growth hormone.
HIIT stimulates mitochondrial growth, improves cellular energy production, and accelerates regeneration processes.
Intermittent fasting:
Fasting activates mitochondrial biogenesis and autophagy, helping remove damaged mitochondria and promoting the formation of new ones.
Nutrients and antioxidants:
Omega-3 fatty acids:
Protect mitochondrial membranes and reduce inflammation.
Coenzyme Q10 and L-carnitine:
Support mitochondrial energy production.
Antioxidants (e.g., vitamins C and E):
Reduce damage caused by free radicals.
Cold and heat exposure:
Cold showers or sauna:
Stimulate mitochondrial production and improve stress resilience.
KETOGENIC DIET / NUTRITION
Ketogenic nutrition is a powerful tool for reducing inflammation and insulin resistance while supporting mitochondrial health and energy metabolism. When combined with other healthy habits—such as regular exercise, intermittent fasting, and a nutrient-dense diet—it improves mitochondrial efficiency, reduces chronic inflammation, and supports the body’s natural healing processes.
Why Statin Drugs (Cholesterol-Lowering Medications) May Not Be Right for You
Mechanism, Side Effects, and Limitations of Statins
Statins are medications that lower LDL cholesterol by inhibiting HMG-CoA reductase—an enzyme required for cholesterol synthesis in the liver. This reduces the liver’s production of cholesterol.
When LDL cholesterol is aggressively lowered with statins without addressing the root causes of vascular damage and chronic inflammation, the result may be a shortage of “repair material” (LDL). This can impair the body’s ability to repair damaged blood vessels, as LDL is needed to patch and restore vascular injury.
Limitations and Side Effects of Statins
Limitation: They do not address the root cause
Statins lower LDL but do not repair blood vessel damage or reduce inflammation. This may be dangerous, as there may not be sufficient material to repair vascular “lesions.”
Medication goals vs. natural body balance:
Excessive LDL lowering may disrupt natural healing processes in which LDL plays a role in endothelial repair and maintaining cell membrane stability.
Potential side effects:
Neurological issues:
Associations with memory loss, Alzheimer’s disease, and increased dementia risk. Cholesterol is essential for brain cell function and nerve signal transmission. Lower cholesterol levels may impair memory and cognitive performance.
Muscle problems:
Muscle pain, weakness, and in rare cases rhabdomyolysis (muscle breakdown). Muscles are crucial longevity organs—the stronger and more developed they are, the better quality and length of life.
Hormonal effects:
Cholesterol is the precursor for sex hormone synthesis, and artificially lowering it may cause hormonal imbalances.
Bone density loss:
Research suggests that suppressing cholesterol synthesis negatively affects bone health.
Cancer risk:
Recent studies indicate that statins may increase cancer risk, particularly breast cancer.
Statin Alternatives: Focus on Root Causes
Instead of statins, focus on reducing inflammation and oxidative stress—the primary drivers of vascular damage. Low-carbohydrate nutrition, physical activity, and stress management are effective strategies for regulating LDL and maintaining vascular health.
Alternatives include:
- Reducing inflammation and insulin resistance
- Monitoring metabolic markers rather than LDL alone
Anti-inflammatory approaches:
Anti-inflammatory medications:
Some studies suggest that inflammation-targeting drugs (e.g., canakinumab) may reduce cardiovascular risk even without lowering cholesterol.
CRP monitoring:
Tracking inflammatory markers such as CRP provides a better assessment of cardiovascular health than LDL alone.
Metabolic Markers – What They Are and Why They Matter
Metabolic markers are biological indicators that reflect the state of metabolism. They help assess health status, predict chronic disease risk, and monitor treatment response. Unlike LDL alone, metabolic markers provide a comprehensive view of overall health.
Key metabolic markers:
1. CRP (C-reactive protein)
Measures inflammation. Elevated levels indicate chronic inflammation linked to cardiovascular disease.
2. Triglycerides
Reflect fat levels in the blood. High levels indicate insulin resistance and metabolic dysfunction.
3. HDL cholesterol (high-density lipoprotein)
The “good” cholesterol that removes excess cholesterol from tissues. Low levels increase atherosclerosis risk.
4. Fasting insulin
High levels indicate insulin resistance, linked to diabetes and cardiovascular disease.
5. Blood glucose and HbA1c
Measure short- and long-term glucose control. Elevated levels indicate diabetes or prediabetes.
6. Lipoprotein particle size and density
Small, dense LDL particles are more atherogenic than large LDL particles.
7. Blood pressure
Reflects vascular stress and chronic inflammation risk.
8. Homocysteine
An amino acid linked to B-vitamin metabolism. High levels increase cardiovascular and inflammatory risk.
Why Focus on Metabolic Markers?
- Holistic assessment: More informative than LDL alone
- Identifies true root causes: Inflammation and insulin resistance
- Personalized approach: Helps determine effective lifestyle and treatment strategies
About the Author – Annika Urm
Annika Urm is an international health, nutrition, and lifestyle consultant, a medical college student, a mother of two, and holds three university degrees, including a Master’s degree in Financial Management.
You can read more about Annika Urm here. She is the creator of the sugar-free keto world and helps people heal and manage conditions such as diabetes, dementia, and Alzheimer’s disease.
Annika Urm is the author of two sugar-free cookbooks, a motivational speaker, and a healthy keto coach.
Low Carb and Keto Diet for Diabetes: The Best Treatment for Many Diseases, Including Diabetes
🔗 https://news.annikaurm.com/2023/11/14/science-based-low-carb-and-keto-diet-for-diabetes-the-best-treatment-for-many-diseases-incl-diabetes
ORDER now:
Keto, Low Carb, Sugar-Free Private Chef- Annika Urm
https://goldenstevia.com/product/keto-low-carb-cook-private-chef-annika-urm
Low Carb, Keto diet menu, personal + 14 day consultation
https://goldenstevia.com/product/low-carb-keto-diet-menu
1h general consultation
https://goldenstevia.com/product/1h-general-consultation-annika-urm
Latest News:
- How to Start Sugar-Free Lifestyle: Step-by-Step Low Carb & Keto Guide with Annika Urm
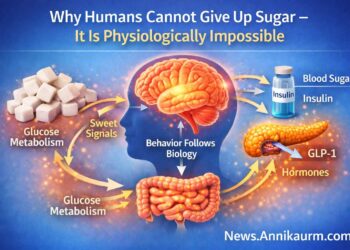
- Why Humans Cannot Give Up Sugar – It Is Physiologically Impossible
- Cholesterol and Inflammation – What Really Causes Vascular Disease?
- How the body really works: the truth about carbohydrates, insulin, fats, keto metabolism
- Daily 15-Minute HIIT Workout, Earthing, and Breath Exercises with Annika Urm