Many people confidently say today: “I do not eat sugar.”
In practical work with people, this statement rarely reflects biological reality. A recurring pattern appears repeatedly. A person decides to remove sugar from daily life and usually interrupts the attempt within one to three days. Individuals with higher motivation and mental endurance continue longer, yet even in these cases the typical duration reaches two to three weeks, followed by a return to previous patterns. This pattern appears consistently across different groups, including metabolically healthy individuals, people with diabetes, and women during the menopausal transition (perimenopause).
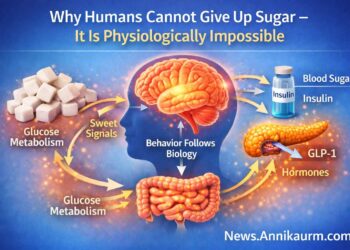
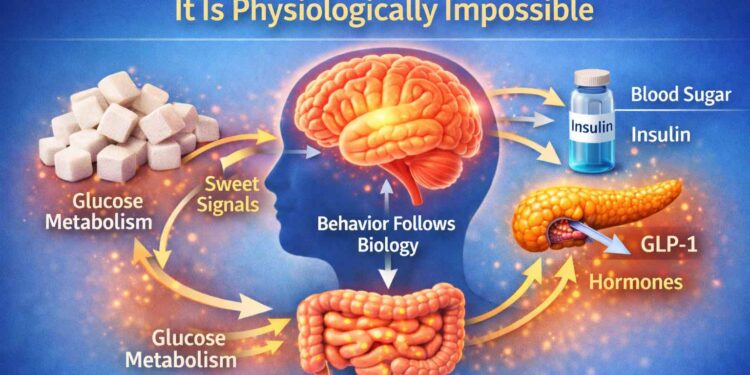
The human body follows biology, not motivation.
Sugar-related behavior is regulated by hormones, brain signaling, and the nervous system.
These systems operate automatically and prioritize energy stability and survival.
“I Do Not Eat Sugar” – Why This Statement Rarely Reflects Reality
People often say this honestly. Cakes, candy, and sweetened drinks are removed from the menu, creating the belief that sugar intake has ended. A closer look at daily eating shows a different picture. Bread, sweet marinades, honey, pasta, potatoes, and grain-based foods often remain. These foods are rarely perceived as sugar, yet in the body they act in the same way.
Biologically, all of these foods are sources of glucose. For the body, the result is the same.
The brain receives a glucose-based sweet signal even from foods that are not perceived as sweet.
The human body does not differentiate whether glucose enters the bloodstream from a spoon of sugar or a slice of bread. During digestion, all of these foods break down into the same end product: glucose. Blood glucose and insulin responses follow the same biological mechanism, regardless of how the food is labeled in the mind. This is where the most common form of self-deception appears. The person does not lie consciously but truly believes they live without sugar, while metabolism continues to receive glucose every day. On a biological level, sugar elimination has not occurred; only the form of sugar has changed.
Why Sugar Elimination Usually Ends Within One to Three Days
The inability to give up sugar does not reflect a lack of willpower or poor habits. It represents a natural physiological response based on biological regulation of the nervous system and metabolism. Sugar elimination rarely begins during a stable state. The decision usually appears when the body already experiences metabolic and neurohormonal strain, including persistent fatigue, weight gain, blood glucose fluctuations, anxiety, sleep disruption, insulin resistance, or type 2 diabetes. During the menopausal transition, reduced estrogen further influences nervous system balance and emotional regulation.
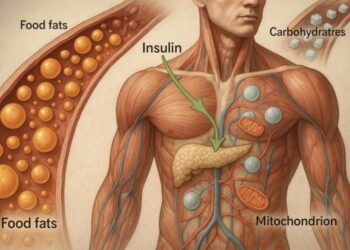
At the hormonal level, chronically elevated insulin plays a central role. Insulin regulates blood glucose while directing energy storage and usage. Sustained insulin elevation maintains glucose-centered metabolism. At the same time, leptin signaling often loses clarity, preventing the brain from receiving accurate information about available energy. The result is a state where eating continues, yet physiological satisfaction does not appear.
Sweet Taste Receptors – What Is Actually Missing
The human body contains specific sweet taste receptors, scientifically known as T1R2 and T1R3. These receptors exist not only on the tongue, but also in the digestive tract and pancreas. This shows that sweetness functions as a biological signal, not only as a taste sensation. Sugar and rapidly glucose-forming carbohydrates activate these receptors and influence brain signaling, hormones, and the autonomic nervous system. Receptor activation supports GLP-1 and GIP release and stimulates insulin secretion, which acts as a central signal hormone for metabolism and energy use.
When sweet receptors activate, neural signaling reaches the brain and stimulates the mesolimbic dopamine pathway (VTA → nucleus accumbens → prefrontal cortex). Dopamine does not represent happiness. It functions as a motivation and repetition signal. The brain receives the message that the situation is safe and valuable.
Important: this signal does not depend on calories.
The brain responds to sweet taste signaling, not glucose alone.
When both sugar and sweet taste disappear simultaneously, this system remains unstimulated. The brain interprets this state as resource insufficiency, not as a healthy choice. Subjectively, this appears as restlessness, irritability, reduced concentration, and a strong desire for “something.” This explains why elimination typically interrupts within one to three days.
The Role of Wheat – Why the Issue Extends Beyond Sugar
Wheat does not function only as a carbohydrate source. During digestion, gliadin, a wheat protein component, breaks down into opioid-like peptides (gluteomorphins). These compounds activate µ-opioid receptors in the brain, creating calming and reward-related signals.
This explains why many people say:
“I do not want sweets, but bread feels difficult to remove.”
This response reflects neurochemical signaling, not habit or personality.
Why Low-Carb and Ketogenic Diets Work for Sugar Cravings and Blood Sugar Stability
Low-carb and ketogenic diets support the body by stabilizing blood sugar and reducing chronically elevated insulin levels. Stable blood glucose plays a central role in reducing sugar cravings and supporting metabolic balance. When insulin signaling becomes calmer, fat utilization increases, inflammatory signaling decreases, and energy regulation becomes more flexible. Many people experience more stable energy, improved mental clarity, and reduced sugar cravings within the first weeks.
However, blood sugar control alone does not guarantee long-term success. When a diet removes both sugar and sweet taste signaling, the nervous system does not receive complete regulatory input. The human brain has evolved to associate sweet taste with energy availability and safety. When this signal disappears abruptly, the brain interprets the situation as energy insecurity, even when caloric intake remains sufficient.
This explains why people following low-carb or ketogenic diets may report reduced hunger but persistent sugar cravings, restlessness, or food thoughts. This response does not indicate dietary failure This response reflects incomplete sweet taste signaling, even when blood sugar and insulin levels remain stable.
When sweet taste signaling disappears entirely, the nervous system pushes back, even in ketosis.
Why the Brain Needs All Five Tastes – Sweet, Salty, Sour, Bitter, and Umami
The human brain does not regulate eating based on calories alone. Appetite control depends on taste signaling, which informs the nervous system about safety, nutrient availability, and balance. The brain requires all five primary tastes to receive complete regulatory input: sweet, salty, sour, bitter, and umami.
Sweet taste signals immediate energy availability and supports stress regulation.
Salty taste supports electrolyte balance and nervous system stability.
Sour taste supports digestion and gastric signaling.
Bitter taste activates protective and regulatory pathways linked to detoxification and digestive readiness.
Umami taste signals protein intake and supports long-term satiety.
When these taste signals are present together, the brain receives clear feedback that nutritional needs are met. When one or more taste signals are missing, especially when sweet taste is removed entirely, the nervous system remains alert and continues to seek resolution, even when food intake is sufficient.
Taste signaling forms the link between food intake and hormonal satiety mechanisms. Without complete taste input, appetite-regulating systems remain partially active, and downstream satiety hormones cannot reach full effectiveness.
GLP-1 and CCK – the Body’s Own “Natural Ozempic”
Low carb and ketogenic diets activate GLP-1 and CCK hormones that regulate appetite naturally. GLP-1 slows gastric emptying, increases satiety, and reduces appetite signaling in the brain. CCK sends a clear “enough” signal during eating. These hormones activate primarily through the combined effect of fat and protein. Protein alone does not produce the same response. This explains why meals like “dry chicken breast and salad” fail to create lasting fullness, as hormonal signaling remains weak and appetite returns. When meals include fat, protein, and fiber, the body regulates intake automatically.
GLP-1 signaling develops over time. Initial activation begins within days to weeks, while stronger and more stable effects appear over several weeks to months as metabolic adaptation progresses.
In some cases, GLP-1 signaling activates more slowly even when food choices remain consistent. This typically relates to long-standing insulin elevation, high baseline carbohydrate exposure, disrupted sleep, chronic stress, or prolonged metabolic inflexibility. In these situations, daily intake alone does not immediately translate into hormonal response. As insulin signaling calms and metabolic flexibility improves, GLP-1 responsiveness increases gradually, and appetite regulation becomes more noticeable and stable.
How to Recognize When GLP-1 and CCK Are Active?
GLP-1 and CCK activity becomes noticeable through physical satiety, not mental control. One clear indicator appears when eating protein- and fat-rich foods. Attempting to eat four eggs or four avocados typically leads to strong and early fullness. For most people, finishing this portion feels physiologically difficult due to satiety rather than willpower.
Another sign involves post-meal stability. Energy remains even, focus stays clear, and the urge to continue eating fades naturally. The body communicates completion clearly during the meal, and eating slows on its own.
As GLP-1 and CCK signaling strengthens over time, portion size adjusts automatically. Longer pauses between meals appear naturally, including intermittent fasting or OMAD (one meal a day), guided by hormonal regulation rather than conscious restriction.
At a certain point, a person notices that finishing all planned food even feels difficult. This is a clear signal that satiety hormones are active. The practical recommendation is simple: eat first what the body truly needs, and only afterward, if appetite remains, eat what is desired. In the early phase, this does not work smoothly, because carbohydrate dependence and established habits still guide food choices.
Conclusion – Appetite Regulation as a Physiological Process
Appetite regulation reflects coordinated brain, gut, and hormonal signaling, not discipline. When taste signaling, GLP-1, and CCK align under low carb and ketogenic nutrition, eating behavior organizes itself through physiological feedback. Satiety becomes clear, portion size stabilizes, and meal timing adapts naturally.
With sustained metabolic adaptation, the body prioritizes nutrient-dense intake, maintains stable energy, and supports flexible eating patterns such as intermittent fasting and OMAD (one meal a day). This state represents efficient cooperation between metabolism and the nervous system, guided by internal signals that support long-term balance.
Low Carb Solution: Changing the Source of Sweetness Without Raising Blood Sugar
This is where we reach the solution that makes low carb and ketogenic diet nutrition truly sustainable. Humans do not require sugar, but they do require sweet taste signaling. This signal can be provided without raising blood glucose or insulin.
Stevia, monk fruit (Luo Han Guo), and erythritol activate sweet taste receptors (T1R2/T1R3) located on the tongue and in the digestive tract. These sweeteners provide the brain with sensory information of sweetness without significant impact on blood glucose or insulin levels. The key factor is that the sweet signal is delivered without a glucose load.
- Monk fruit – sweetness comes from mogrosides, which do not metabolize into glucose
- Stevia – steviol glycosides provide sweet taste signaling without glycemic load
- Erythritol – partially absorbed and largely excreted unchanged
Biological outcome: the brain receives a calming and stabilizing signal while metabolism remains stable. As a result, compulsive behavior decreases, cravings fade naturally, and low carb or ketogenic nutrition becomes sustainable rather than a willpower-based project. This represents a physiologically normal state for the body.

https://goldenstevia.com/product-category/sweetener
Buy here: 100% Natural Monk Fruit sweetener pure Luo Han Guo extract V 3,5%
https://goldenstevia.com/product/100-natural-monk-fruit-sweetener-pure-luo-han-guo-extract

Berries, Fruit, and Honey – When Sweetness Is Appropriate
Sweetness itself is not the problem. The question is not whether sweetness is “allowed,” but for whom and in which metabolic state. A healthy, metabolically stable individual with balanced blood sugar and a functioning inhibitory system can consume berries, fruit, and honey in reasonable amounts without triggering loss of control. Such a person has intact internal brakes. Satiety develops, appetite settles naturally, and sweetness does not become obsessive. For this individual, honey or berries remain a food component, not a trigger.
The situation changes when a person is carbohydrate-dependent. In this state, the issue is not the food itself, but neurochemistry. When the inhibitory system is weakened, portions do not remain moderate. “A little honey” quickly turns into “a bit more,” followed by bread, pasta, or processed sweet foods. This reflects dopamine and insulin interaction, which overrides inhibitory signaling. This process relates to physiology, not personality.
For this reason, the same dietary recommendations do not apply to everyone. A metabolically healthy individual can include sweetness from berries and honey. A carbohydrate-dependent individual cannot begin there, as this approach carries excessive risk.
Processed Sweet Foods – Why They Disrupt Appetite Regulation
It is important to distinguish natural sweetness from processed sweetness. Processed sweet foods are not simply sugar. They represent a combination of refined carbohydrates, fats, salt, and flavor enhancers, designed to produce a strong dopaminergic response in the nervous system.
Foods from supermarkets such as cakes, candies, soft drinks, sweet pastries, and fast food do not provide the body with nutritional signaling. Instead, they overstimulate the nervous system. The brain does not receive a signal of completion, but a signal to continue. As a result, intake does not stop naturally after one portion.
Processed sweetness is not neutral, regardless of whether a person follows low carb or ketogenic nutrition. This explains why processed sweet foods most rapidly reactivate previous cravings and relapse patterns, even after periods of metabolic stability.
Artificial Sweeteners in Processed Foods – An Important Distinction
A clear distinction is required when discussing artificial sweeteners in processed foods. Sweeteners such as aspartame, acesulfame-K, sucralose, maltitol, and sorbitol interact with the body through different neurochemical mechanisms than natural sweeteners.
Stevia and monk fruit are not comparable to aspartame. Many commercial products labeled as “stevia-based” contain blended formulations, which explains why some individuals report unpleasant taste perception or physical discomfort. These reactions are related to formulation, not to stevia itself.
Pure stevia and pure monk fruit, such as those used in Golden Stevia products, differ in composition and physiological response. They align with low carb and ketogenic nutrition practices and support sweet taste signaling without disrupting blood sugar or insulin regulation.
Conclusion – Appetite Regulation Is a Physiological Process
Humans Cannot Give Up Sugar – It Is Physiologically Impossible
Humans cannot give up sugar because appetite regulation is governed by physiology, not willpower. The human brain, hormonal system, and nervous system require continuous sweet taste signaling to maintain metabolic stability and perceived energy security. This mechanism operates automatically and supports survival-based regulation.
Sweet taste signaling, blood glucose balance, insulin activity, and gut–brain hormones such as GLP-1 and CCK function as a unified biological system. When these signals align, appetite regulation becomes stable, satiety develops naturally, and eating behavior organizes itself without conscious restriction.
This explains why complete sugar removal does not match human physiology, while changing the source of sweetness supports long-term balance. When sweetness comes from non-glycemic sources such as stevia and monk fruit, the brain receives the required sensory input while blood sugar and insulin remain stable.
In this physiological state, cravings settle, portion size stabilizes, and low carb or ketogenic nutrition becomes sustainable. The solution is not eliminating sweetness, but aligning sweet taste signaling with the body’s natural regulatory systems.
Appetite regulation reflects coordinated brain, gut, and hormonal signaling rather than conscious control. When low carb or ketogenic nutrition supports stable blood sugar, insulin balance, and sweet taste signaling, the body organizes eating behavior through physiological feedback.
In this state, low carb nutrition functions as a normal metabolic condition, not a restrictive intervention. The body and nervous system operate in cooperation, guided by biological regulation that supports long-term balance and sustainability.
Golden Stevia – Sugar-Free, Keto and Low Carb Sweeteners and Baking Products
Recommended product
Sugar replacement 1:10 with stevia and inulin for low carb, keto, and sugar-free cooking and baking.
Golden Stevia Inulin Sweetener Powder 1:10 is a high-strength sugar replacement, where 500 g replaces 5 kg of sugar.
- 1:10 sugar replacement with natural sweet taste
- 500 g equals 5 kg of sugar
- Stevia and chicory root inulin for keto and low carb baking
Golden Stevia is a specialized low carb and keto online store offering sugar-free, gluten-free and diabetic-friendly sweeteners and baking products. The product range focuses on pure stevia and pure monk fruit sweeteners, as well as keto and low carb baking mixes designed to support sweet taste signaling without raising blood sugar or insulin.
Golden Stevia sweeteners activate T1R2 and T1R3 sweet taste receptors, allowing GLP-1 and CCK signaling to remain stable while maintaining metabolic balance. This makes Golden Stevia products suitable for low carb, ketogenic, sugar-free and diabetic-friendly nutrition, without compromising taste or physiological regulation.
The Golden Stevia online shop brings together sugar-free sweeteners, keto baking mixes, low carb ingredients and gluten-free products in one place, making it easier to enjoy familiar foods such as keto bread, pizza, pastries and desserts while following a low carb lifestyle.